More specialist clinics would reduce numbers with Type 2 Diabetes

Wed, 14 Sep 2016 12:28:00 BST
New research shows type 2 diabetes could be slashed by 80% if more was done to encourage people with “pre-diabetes” diagnoses to change their lifestyles
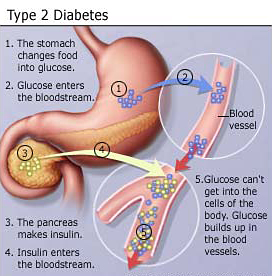
 IT is estimated that the treatment of diabetes costs the NHS in England and Wales more than £1.5m an hour – 10 per cent of its budget. Numbers of people diagnosed with the disease have risen to 3.5 million. But the numbers developing type 2 diabetes – the most common form – could be slashed by 80 per cent if people at risk made lifestyle changes. Researchers at the University of Huddersfield believe that “pre-diabetes” diagnoses and special clinics could bring about this massive reduction. Now, they aim to establish the best way to achieve it.
IT is estimated that the treatment of diabetes costs the NHS in England and Wales more than £1.5m an hour – 10 per cent of its budget. Numbers of people diagnosed with the disease have risen to 3.5 million. But the numbers developing type 2 diabetes – the most common form – could be slashed by 80 per cent if people at risk made lifestyle changes. Researchers at the University of Huddersfield believe that “pre-diabetes” diagnoses and special clinics could bring about this massive reduction. Now, they aim to establish the best way to achieve it.
Dr Warren Gillibrand (pictured left) – a Senior Lecturer in the University’s Division of Podiatry and Clinical Science – has widespread experience of diabetes care and research. With University of Huddersfield colleague Stephen Phillips and York-based district nurse Wendy Youngs, he has authored a new article that examines the impact of pre-diabetes diagnosis and whether it is effective in bringing about the necessary changes in lifestyle.
The article’s findings are that pre-diabetes is a “challenging concept for patients and nurses alike”, and more education and support are required to motivate lifestyle change in the person at risk.
“This, however, does not need to be medicine led; use of peer and community-based programmes could be not only cheaper, but also have the ability to provide potentially long-term support for people, and would provide continued reduced risk,” state the authors.
 “Intervention needs to ensure that it is provided at an appropriate level to account for cultural, social and gender needs. Innovative approaches need to be considered to reduce the number of people who are diagnosed with pre-diabetes from progressing to type 2 diabetes and its associated potential complications.”
“Intervention needs to ensure that it is provided at an appropriate level to account for cultural, social and gender needs. Innovative approaches need to be considered to reduce the number of people who are diagnosed with pre-diabetes from progressing to type 2 diabetes and its associated potential complications.”
Dr Gillibrand said that studies in Scandinavia had shown that the 80 per cent reduction in type 2 diabetes is achievable, and that pre-diabetes clinics are now widely established in NHS trusts.
“People identified as being at high risk are mainly referred to the clinics by a GP, based on a number of different factors, such as lifestyle, weight, smoking history and biochemical markers,” he explained.
 A range of interventions have been developed, based around patient education.
A range of interventions have been developed, based around patient education.
“However the arguments in the article are that education alone in its purest form probably isn’t that effective,” said Dr Gillibrand. “There is a need for other mediators – for example behaviour interventions or talking-based psychological therapies in order to initiate lifestyle change.”
After publishing their initial findings, Dr Gillibrand and his co-researchers now aim to secure funding for a large-scale evaluation of pre-diabetes clinics and the different models of educational programme. There are also regional factors to be examined, with some areas more likely to have pockets of the population at risk of developing diabetes.
Dr Gillibrand estimates that his evaluation project would probably last two years and require funding of £350,000. At least four NHS trusts in contrasting areas would need to be involved, in order to obtain meaningful data.
“The ideal output would be to make the case for pre-diabetes clinics and to support the argument that Department of Health need to provide greater levels of funding,” he said. “After all, the prevention of type two diabetes is a national priority.”
- “The impact of pre-diabetes diagnosis on behaviour change: an integrative literature review” by Wendy Youngs, Warren P. Gillibrand and Stephen Phillips is in Practical Diabetes International, 33 (5).